The Brain's Energy Crisis and Why It Matters
Why does your brain fog up when you're tired, stressed, or recovering from illness? The human brain presents a metabolic paradox: it comprises just 2% of body weight yet consumes 20% of the body's oxygen and approximately 25% of its glucose. In children, this figure rises to 50% of whole-body oxygen consumption during peak developmental years. This extraordinary energy demand makes neurons uniquely vulnerable to mitochondrial dysfunction—when cellular power plants fail, cognition falters first. Think of it like brownouts in a city grid; the most energy-intensive districts lose power before anything else.
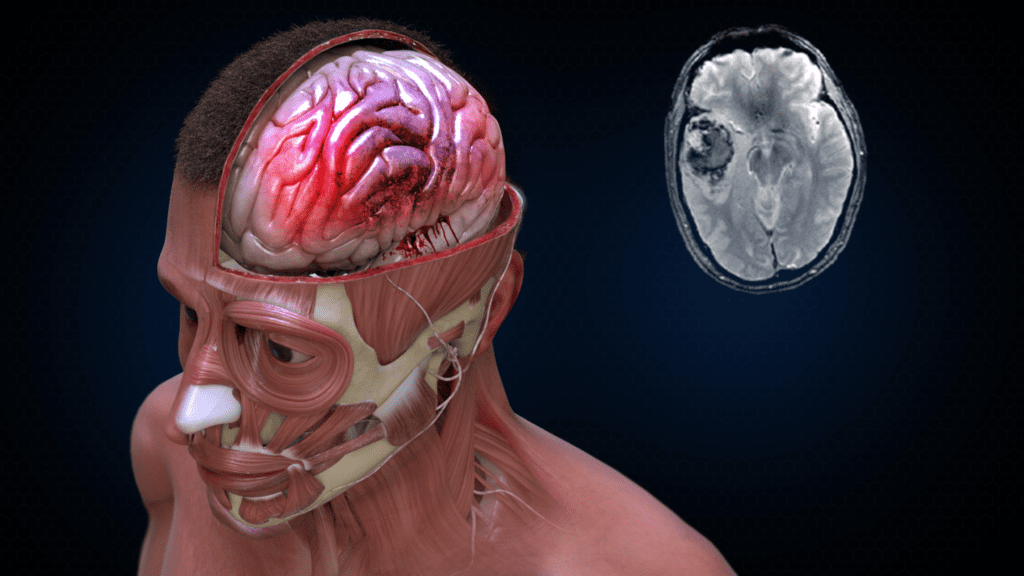
The brain's disproportionate energy demands make it uniquely vulnerable to mitochondrial dysfunction
What happens when mitochondria stop working properly? Under normal conditions, oxidative phosphorylation produces 32-36 ATP molecules per glucose molecule, fuelling everything from memory consolidation to executive function. When mitochondria become impaired through infection, stress, ageing, or toxin exposure, cells fall back on anaerobic glycolysis—producing just 2 ATP per glucose molecule, a potential 94% reduction in cellular energy output. Research published in the European Journal of Neurology systematically documented how adult mitochondrial disease manifests cognitively: processing-speed problems at the neuronal level, progressively worsening neuropsychological performance, and deficits across visuospatial functioning, memory, attention, and executive function. It's kinda like switching from mains electricity to a single AA battery.
Does this pattern hold across different conditions causing brain fog? The pattern is consistent across conditions. A 2023 National Institute on Aging study demonstrated that lower mitochondrial function in skeletal muscle increases the risk of mild cognitive impairment or dementia in older adults, establishing links between mitochondrial dysfunction and brain amyloid plaques. For Long COVID patients specifically, a 2025 prospective case-controlled study published in the Annals of Medicine found impaired mitochondrial function in peripheral blood mononuclear cells, with researchers describing ATP synthase running both forward and reverse reactions—a metabolic signature of chronic energy crisis. The mitochondrial hypothesis for cognitive fatigue isn't speculative; it's documented across multiple pathologies.
Energy Production Comparison
| Metabolic State | ATP per Glucose | Cognitive Impact |
|---|---|---|
| Healthy mitochondria | 32-36 ATP | Normal cognition, sustained focus |
| Impaired mitochondria | 2 ATP | Brain fog, fatigue, processing delays |
| Energy reduction | 94% loss | Severe cognitive impairment |
What does this mean for practical intervention strategies? If brain fog stems from an energy crisis at the cellular level, then interventions must address mitochondrial function directly rather than masking symptoms with stimulants. This is where methylene blue's mechanism becomes relevant—it targets the electron transport chain itself, potentially bypassing damaged complexes to restore ATP production. The question isn't whether mitochondrial dysfunction causes brain fog (the evidence is overwhelming), but whether methylene blue can effectively reverse it in humans experiencing cognitive fatigue.